July 15, 2019by marketanggroupdev
Endoscopic Discectomy Procedure
If you are looking for relief from pain caused by a herniated disc and low back pain, an endoscopic discectomy could be the answer you need. This is the least-invasive procedure performed in our outpatient surgical facility that removes herniated disc material. Endoscopic spine surgery is considered least-invasive. Least-invasive surgeries (LIS) offer many benefits that traditional spine surgeries do not. Traditional surgeries often require long recovery times and have high infection and morbidity rates. LIS decreases the risks involved with surgery, reduces recovery time, and returns most patient to work within two to three weeks. It’s important to talk to your doctor about the benefits and risks of endoscopic spine surgery to determine if it’s the right choice for you.
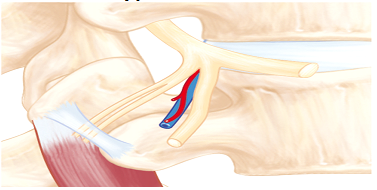
Endoscopic discectomy is different from open or MIS lumbar microdiscectomy. In our endoscopic spine surgery, there is no muscle dissection, no removal of the bone, and we don’t need to make a large incision in your skin. Because of that, there is less risk of scarring, infection, blood loss, or complications from anesthesia. Endoscopic discectomy was invented as a least-invasive interventional pain management procedure that effectively treats herniated discs while lowering the risks involved with traditional surgeries.
The advantage of an endoscopic spine procedure is that your surgeon only needs to make a ¼ inch incision. That means the muscles of the middle of your back are spared, which results in less recovery time and fewer risks for complications.
HOW IS THE PROCEDURE PERFORMED?
You’ll be given a local anesthetic so you don’t feel anything during the surgery. Once you’ve been numbed, an incision will be made near the herniated disc and through muscle tissue in your back. A dilator is inserted to keep the incision open with a 1/4 inch metal tube giving the surgeon access to the disc. An HD camera/endoscope is inserted so the surgeon can clearly see the herniated disc and make an evaluation of what needs to be removed. Microscopic instruments are inserted through the endoscope to remove the herniated disc. Inside of the disc, any tears are cleaned and treated with a laser to ablate the nerves that are growing in the tear of the annular layer of the disc. The laser shrinks and closes the tears while keeping the disc intact. Once the treatment is complete with any tears sealed and herniated discs removed, the metal tube is taken out and the surgeon will close the incision.
ADVANTAGES OF ENDOSCOPIC DISCECTOMY INCLUDE:
- 90% or higher success rates
- HD cameras are used to give the surgeon a better view of the damage in the area
- No spinal fusion is necessary
- Minimal incision size of just 1/4 inch reduces the risk of scarring
- Spinal mobility is preserved because there is less scarring and tearing of muscle tissue
- Less risk for large amount of blood loss
- Conscious sedation means there is no need for general anesthesia
- Less recovery time
- Less pain during recovery means less dependence on narcotic pain medication
- You can resume normal activities sooner!
WHAT IS THE ENDOSCOPIC DISCECTOMY SUCCESS RATE?
Published follow-up studies and our in-house observations show that endoscopic discectomy surgery is a highly successful procedure. A study that observed the post-surgical condition of patients over a 10-year period showed that more than 80 percent reported excellent results and none had any poor results.
WHAT IS THE ENDOSCOPIC DISCECTOMY RECOVERY TIME?
The time of recovery for the endoscopic discectomy procedure depends on the type of work you do.
For people who do office work and other kinds of sedentary jobs, the time of recovery is usually one to two weeks. For more active people, like athletes and those who move around more often during their regular workday, the time of recovery may be four to six weeks.
During the recovery period, you’ll need to participate actively in a physical therapy program. Physical therapy will help you recover and return to your regular activities faster. Some patients may also be required to take pain relievers during the recovery period.
HOW LONG IS THE RECOVERY AND HOW SOON CAN YOU RETURN TO WORK?
An endoscopic discectomy takes about an hour. You shouldn’t experience a great deal of pain afterward but may feel a little sore. You don’t even have to worry about stitches; your incision will simply be covered with a band-aid. It takes about an hour to recover from the procedure in our outpatient surgical facility and then you can go home. After that, you’ll need to see how your body responds to the surgery. Most patients feel better right away and can return to work in a couple days. It’s important to listen to your body and discuss your symptoms with your doctor to ensure you are ready to resume normal activities. Avoid heavy lifting until your doctor gives you the okay, even if you feel fine.

July 15, 2019by marketanggroupdev
Endoscopic Foraminoplasty
What Conditions Does Endoscopic Foraminoplasty Treat?
The endoscopic foraminoplasty is one of the least invasive spine surgeries. It is used to relieve pressure on the exiting nerve or spinal cord, caused by:
The last three conditions on this list are caused by a narrowing of the spine or foramen. Using an endoscopic approach, this technique uses microscopic surgical tools through an endoscope to selectively remove some of the bone. This helps enlarge the foramen and relieve pressure on the nerves.
What Is The Endoscopic Foraminoplasty Success Rate?
From our experience at Spine Institute of North America and research studies published on the effectiveness of endoscopic foraminoplasty, we can say that it has a success of rate of over 90 percent.
In a study of 16 patients who went through the endoscopic foraminoplasty procedure, 15 recorded excellent or good outcomes, and none had a poor outcome. There were no post-operational infections or injuries. Also, none of the patients needed a second operation.
WHAT IS THE TYPICAL ENDOSCOPIC FORAMINOPLASTY RECOVERY TIME?
Unlike open spine surgery used to treat foraminal stenosis, endoscopic foraminoplasty surgery uses only a small incision. That’s why, instead of the 12-month recovery period for open spinal surgery, recovery time for this modern surgical procedure is far less dependent on the severity of the pain and condition. In most cases, the patient can start physical therapy the same day as the operation.
How Long Is The Recovery?
he procedure takes about an hour on average. Most patients need about an hour to recover after the surgery, and then they are free to go home. You will have little if any pain or discomfort; in fact, you won’t even have any stitches! The surgeon will simply cover the incision with a small band-aid.
HOW SOON CAN YOU RETURN TO WORK?
Recovery depends on how well you and your body respond to the procedure. Typically, most patients will feel better immediately after surgery and go back to work within a few days. Be careful to listen and comply with your physician’s post-operative instructions. Although you may feel better, it is best to not do any heavy lifting at all until cleared by your physician.
ARE YOU A GOOD CANDIDATE FOR ENDOSCOPIC FORAMINOPLASTY?
To see if you are a good candidate for an Endoscopic Foraminoplasty, take our pain evaluation questionnaire and someone from our office will get back to you within a day.
HOW IS THIS PROCEDURE PERFORMED?
You will be given local anesthesia, after which the surgeon will insert a dilator into a 1/4 inch incision in your back. The incision will be near the herniated disc. Then the surgeon will insert a 7mm tube, keeping the incision open so the surgeon has access to the damaged disc. An HD camera is inserted into the tube so the surgeon can get a good, clear look at the disc in order to see the issue that’s causing your pain. Next, the surgeon will use microscopic surgical instruments to remove the damaged portion of your disc, facet joint, or any scar tissue that might be present and irritating the spinal nerve. The surgeon can also use a last and radiofrequency probe to decompress the foramen. This will allow the spinal nerve to function again and relieve many painful symptoms you may have been experiencing.
Advantages Of Endoscopic Foraminoplasty Vs. Transforaminal Lumbar Interbody Fusion (TLIF)
- An HD camera is used to give the surgeon a better view of the disc damage as compared to traditional surgical methods
- No need for a spinal fusion
- Uses a tiny incision so there is less risk of scarring
- Spinal mobility is preserved thanks to less scarring
- Small incision eliminates the risk of significant blood loss
- No need for general anesthesia
- Less pain after the procedure, reducing the need for narcotic painkillers
- Less recovery time needed so patient can resume normal activities sooner
- Patients can get back to work sooner

July 15, 2019by marketanggroupdev
Endoscopic Laminotomy
For patients with lumbar spinal stenosis (LSS) who have not responded to conservative treatment, there is another option before you pursue an invasive spine surgery. An endoscopic laminotomy is a minimally invasive spinal procedure that could effectively treat your symptoms, whether they are from LSS or some other spinal condition, and provide you with much-needed relief.
Almost everyone will experience some kind of spinal degeneration as they age. Lumbar spinal stenosis occurs when the spinal canal becomes narrowed. This could happen because of age or some other spine-related issue like bone spurs or herniated discs. When the spinal canal narrows, it puts pressure on the spinal nerves causing a host of adverse side effects such as back pain, leg pain, numbness or tingling, as well as other symptoms.
A traditional laminotomy is a decompressive surgical procedure that relieves pressure on the nerves and gives them more space in the spinal column by removing part of the lamina, the bony arch of the vertebra that protect the spinal cord, as well as bone spurs, herniated disc material or fatty ligaments. However, an endoscopic laminotomy is one of the least invasive surgeries for effective treatment of LSS and may provide patients with the same benefits.
What Is An Endoscopic Laminotomy?
The team at Spine Institute of North America seeks to provide conservative treatment options for lumbar spinal stenosis first and foremost. However, if these fail to treat your symptoms, your doctor may recommend an endoscopic laminotomy.
When you undergo an endoscopic laminotomy, you’ll be able to leave the surgical center the same day the procedure is performed. After being sedated, your skin is numbed, and a small incision no bigger than two centimeters is made in the target area. Generally, an X-ray taken ahead of time will allow your doctor to verify where this incision needs to be made.
During the procedure, the surgeon creates an opening of the lamina above and below the spinal disc to relieve nerve compression. If some of your pain is caused by a herniated disc, then the surgeon can also address this concern at the same time.
What Conditions Does An Endoscopic Laminotomy Treat?
An endoscopic laminotomy can help treat the following conditions:
WHAT IS THE SUCCESS RATE FOR AN ENDOSCOPIC LAMINOTOMY?
At Spine Institute of North America, our patients have achieved overwhelming success in the relief of adverse symptoms associated with lumbar spinal stenosis through this procedure. Our results are confirmed by research showing that almost all patients who undergo an endoscopic laminotomy report a significantly lower level of disability and pain severity after the procedure is complete.
Who Is A Candidate For This Procedure?
Endoscopic laminotomies are the perfect solution for those who have exhausted conservative options in the treatment of their LSS and other related conditions. It is minimally invasive, especially when compared to a traditional laminotomy. However, your physician at Spine Institute of North America will examine your specific circumstances before determining if this treatment is right for you.
WHAT ARE THE ADVANTAGES OF AN ENDOSCOPIC LAMINOTOMY?
Some of the advantages you can expect from pursuing an endoscopic laminotomy to treat your condition include:
- Minimally invasive procedure and a shorter recovery time
- Extremely high success rates
- Almost no blood loss, or very minimal loss
- Requires only local anesthesia
- Preservation of spinal mobility
- Requires only a small incision
- Minimal scar formation
- Requires no hospitalization — surgery is an outpatient procedure with patients going home the same day
What Is Recovery Like After An Endoscopic Laminotomy?
An endoscopic laminotomy generally takes just over an hour to complete. Unlike invasive open spine surgery, it’s an outpatient procedure that does not require patients to stay in the hospital. In fact, patients can go home the same day the procedure is performed. Because there is less blood loss, and the surrounding tissue receives less disruption, patients experience far less postoperative pain. This means they don’t require as much pain medication.
Your doctor may recommend postoperative exercises. Also, they will discuss with you as to when you can go back to work and resume your normal level of activity.
FIND OUT MORE AT SPINE INSTITUTE OF NORTH AMERICA
If lumbar spinal stenosis is negatively impacting your life or if you are experiencing adverse symptoms related to your back pain, then it’s time to make an appointment at Spine Institute of North America. Our team of doctors will work with you to find an appropriate treatment that will help you live a fuller and more active life.

July 15, 2019by marketanggroupdev
Endoscopic Rhizotomy
Endoscopic Rhizotomy
An endoscopic rhizotomy is an outpatient procedure that’s one of the least invasive procedures that allows our physician direct visualization of the dorsal ramus branch of nerves including the medial and lateral branch nerves. These nerves innervate the facet joint and connect the pain signal from your back muscles to your brain. When our physician directly observes the nerves with an HD endoscope, he can see and ablate the nerves with certainty and provide significant long-term back and neck pain relief. This least-invasive procedure has significant advantages over the pain management’s percutaneous radiofrequency facet ablation procedure, which is done under a fluoroscopic X-ray.
The endoscopic rhizotomy procedure may be used to treat patients who are suffering from:
- Chronic back pain
- Muscle spasms
- Pain when leaning backward (but leaning forward is fine)
- Patients who experienced temporary relief with a percutaneous medial branch rhizotomy
Patients report better long-term results from this least-invasive procedure, compared to a traditional percutaneous rhizotomy. An endoscopic rhizotomy can effectively treat back pain, spasms, and provide chronic back pain relief.
What Conditions Does Endoscopic Rhizotomy Treat?
- Facet Joint Syndrome
- Failed back surgery
- Facet related arthritis
- Back spasms related to the facet joint
- Chronic low back pain
When Is An Endoscopic Rhizotomy Procedure Recommended?
- If you’ve been experiencing lower back pain for more than six weeks
- You’ve had a percutaneous rhizotomy before but symptoms have returned
- Rubbing your lower back increases spasms
- You’ve experienced pain relief of 50% or more from a medial branch block procedure
How Is The Procedure Performed?
You’ll be given local anesthesia. A tiny incision (about 1/4 of an inch) will be made in the skin and muscle of your back near the facet joint of the vertebrae. A 7mm tube is inserted into the incision so the surgeon can access the medial branch nerve. Next, an HD camera is inserted into the metal tube, which gives the surgeon a high-definition view of the medial branch nerve. Using microscopic instruments, the surgeon will ablate the medial branch nerve.
Once the nerve is treated, the metal tube is extracted. There is no need for a stitch; the surgeon will place a small Band-Aid over your incision.
What Are The Advantages Of Endoscopic Rhizotomy Vs. Percutaneous Radiofrequency Facet Ablation?
- Many patients report long-term relief of three to five years
- Instead of multiple percutaneous procedures, there is just one procedure
- Your surgeon will be able to see the nerves that are causing your pain and target them with ablation
WHAT IS THE ENDOSCOPIC RHIZOTOMY SUCCESS RATE?
From our experience and clinical studies, we can say that endoscopic rhizotomy surgery has been carried out successfully and is effective over a period of three years. This span makes it appropriate for treating back pain caused by arthropathy of lumbar facet joints in which there is no leg pain.
The exact percentage of successes in different studies varies, but the majority of endoscopic rhizotomy treatments we administer are successful.
¿Cuál Es El Tiempo De Recuperación De La Rizotomía Endoscópica?
El procedimiento de rizotomía endoscópica generalmente se realiza de forma ambulatoria. Dentro de una hora después de que se complete el procedimiento, podrá regresar a casa. La recuperación completa de este procedimiento no invasivo de 30 minutos lleva solo unas pocas semanas.
Durante el período de recuperación, se le pedirá que acuda a citas de seguimiento. Se puede realizar fisioterapia para ayudarlo a ganar fuerza y movilidad. También es posible que deba tomar algunos medicamentos para aliviar el dolor para reducir las molestias durante el período de recuperación.
¿Cuánto Dura La Recuperación Y Qué Tan Pronto Puede Volver Al Trabajo?
Este tipo de cirugía de columna endoscópica demora aproximadamente treinta minutos y estará listo para irse a casa después de la cirugía en aproximadamente una hora. Experimentará muy poco o ningún dolor por el procedimiento. Deberá mantenerse en contacto con su médico durante su recuperación para determinar cuándo puede reanudar sus actividades normales. Muchos pacientes se sienten mejor inmediatamente después del procedimiento y pueden volver a trabajar en solo un par de días. Asegúrese de seguir las instrucciones de su médico y evite levantar objetos pesados hasta que haya recibido la autorización médica.